How does the system define in network or out of network visits and how do I change this?
Problem
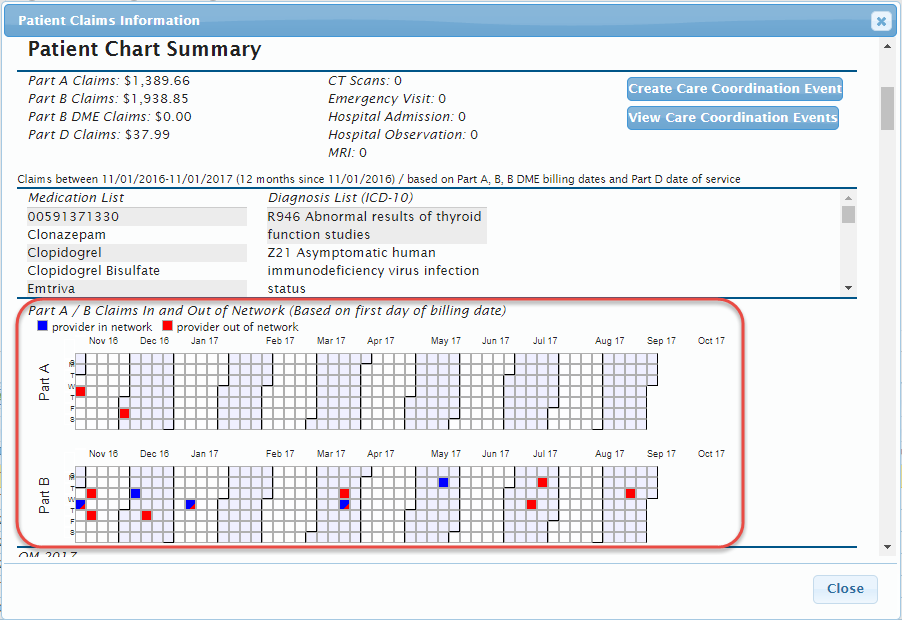
When viewing in network and out of network visits on a patient's claims data, how does the system know which is which? Can this be changed?
Solution
If a TIN and NPI are associated in the system, then claims data relating to this TIN/NPI pairing is considered in network. All other claims data relating to a patient is considered out of network.
To change out of network claims to in network, use the TIN/NPI Management tool to associate the two together.